During puberty, when your body develops from a kid to an adult, many people start thinking and talking about sex. Confused? We’re here to help!
On this page:
Anatomy
First, let’s go over sexual and reproductive anatomy (body parts). We’ve divided it up into what is traditionally called male and female anatomy, although everyone’s genitals are different and are not representative of one’s gender identity.
Male Anatomy
External (outside the body)
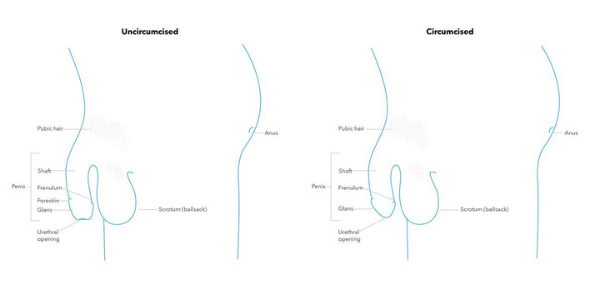
- Penis– the male sexual organ. When a person gets turned on or aroused, the penis fills with blood, causing an erection, or when the penis is “hard.” The average hard penis is 5-7 inches, and some get bigger when hard, and others don’t really change in size. Some penises are circumcised, meaning they had the foreskin removed, and others aren’t.
- Parts of the penis:
- Glans– head/tip of the penis, with the opening of the urethra, where pee/urine and semen leave the body. Also the most sensitive part of the penis for some
- Shaft– the part of the penis from the glans to where it connects to the body
- Foreskin– for those who have not been circumcised, it protects the head and pulls back when the penis is hard to expose the tip
- Frenulum– a small V just below the head, where the foreskin connects to the underside of the penis; very sensitive for most people
- Scrotum– also known as the ballsack, it is the sack of skin that holds the testicles and hangs below the penis. The skin covering the scrotum is wrinkly and covered with hair, and the scrotum is really sensitive.
- Anus– opening to the rectum where feces/poop comes out of, also can be stimulated for sexual pleasure
Internal (inside the body)
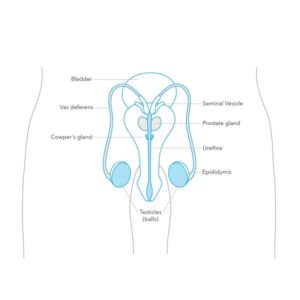
- Testicles (balls)- glands inside of the scrotum that produce sperm and hormones
- Epididymis– tube where sperm matures and connects the testicles to the vas deferens
- Vas deferens– long tube that carries sperm from the epididymis to the seminal vesicles during ejaculation
- Seminal vesicles– two small organs located below the bladder the produce semen, which is the fluid that contains sperm
- Prostate gland– produces a fluid that helps sperm move, and is very sensitive and pleasurable to touch for some people
- Cowper’s glands– produce pre-ejaculate or “precum”
- Urethra– tube that carries urine, pre-ejaculate, and semen to the urethral oening
- Crewmaster– muscle that moves the scrotum and testicles closer to the body
(Source: Planned Parenthood)
Female Anatomy
External (outside the body)
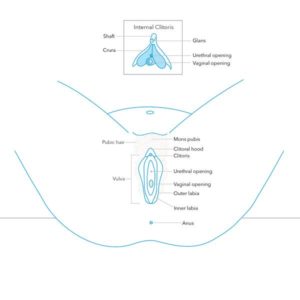
- Mons pubis– skin above the vulva that cushions the pubic bone, and is covered in pubic hair after puberty
- Labia– there are two folds of skin, or lips, around your vaginal opening: the outer labia (labia majora) and the inner labia (labia minora).
- Clitoris– the clitoris is located at the top of the vulva and the tip is covered by the clitoral hood. The clitoris is responsible for sexual pleasure- in other words, it feels good when stimulated during sex or masturbation!
- Urethral opening– the hole that urine or pee comes out of
- Vaginal opening– the hole through which menstrual blood and babies leave the bodies; also where you can insert a tampon/menstrual cup and a partner’s penis, fingers, or sex toys
- Anus– opening to the rectum where feces/poop comes out of, also can be stimulated for sexual pleasure
Internal (inside the body)
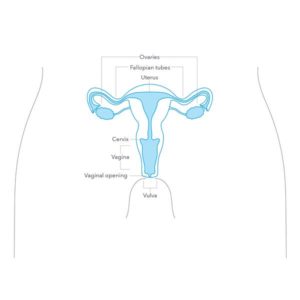
- Vagina– the vagina is a stretchy, muscular tube through which menstrual blood and babies leave the body, and expands when someone is aroused/turned on. Also where you can insert a tampon/menstrual cup and a partner’s penis, fingers, or sex toys
- Cervix– divides the vagina and the uterus, with a small hole through which menstrual blood is released. The opening in the cervix is really small, so tampons and other objects can’t get lost or pass through to the uterus
- Uterus– a muscular organ where a fetus grows during pregnancy
- Fallopian tubes– two tubes, one on each side of the uterus, where the egg travels from the ovaries to the uterus
- Ovaries– the ovaries store you eggs, produce hormones that control your menstrual cycle, and after puberty begin to release an egg once a month
(Source: Planned Parenthood)
How do people become pregnant?
Pregnancy occurs when a person with a penis ejaculates (comes) into a vagina. If the person with the vagina is ovulating, meaning they have released an egg from the ovaries into the fallopian tube, they can become pregnant when the sperm in the ejaculate travel up through the vagina, cervix, and into the fallopian tube to fertilize the egg. The fertilized egg will then travel through the fallopian tube and implant in the uterus, marking the beginning of pregnancy.
You can prevent pregnancy by using barrier methods, like condoms, to prevent the sperm from traveling through the cervix, or different types of birth control that prevent pregnancy through hormonal methods.
You CAN get pregnant from penetrative, penis-in-vagina sex. During this type of sex, you can get pregnant not only from ejaculate (come) but also from pre-ejaculate or precum. You CANNOT get pregnant from oral or anal sex.
The Menstrual Cycle
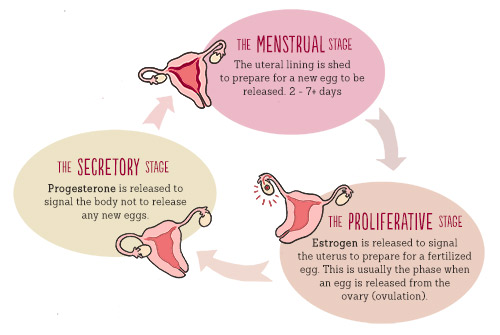
The “menstrual cycle” is the process that your body goes through to prepare for a possible pregnancy. One ovary releases an egg, and the uterus builds up its lining to prepare for a fertilized egg to implant itself. When this doesn’t happen, the uterine lining sheds, resulting in the release of blood through the vagina, or a “period.” The graphic above explains the cycle and the hormones that make it happen.
On average, girls get their first period around the age of 12, but it can happen from the ages of 10-16. The bleeding lasts about 3-8 days, and the menstrual cycle lasts about 28 days, but can range from 21-35 days (or longer). This means, if you have a menstrual cycle that lasts 28 days, you will get your period every 28 days.
Leading up to your period, you might have PMS, or “premenstrual syndrome.” These are the symptoms you may get leading up to your period, due to the hormones in your body. PMS affects everyone differently, but some people may feel bloated, have sore breasts, headaches, mood swings, and more (learn more about PMS here).
During your period, especially during the first few days, you may get cramps as your uterus contracts to expel the uterine lining. These can be really uncomfortable, but they can be managed through over-the-counter (meaning you can get it without a prescription) pain relief drugs like ibuprofen, naproxen, or acetaminophen. Other things that help include exercise, using a heating pad or hot water bottle on your stomach, and taking a hot bath.
There are a few options to collect the blood during your period, depending on what works best for you. They are:
- Pads, which attach to your underwear
- Tampons, which are a small piece of cotton you insert into your vagina with a plastic applicator
- Period underwear, which are specially made to be worn during your period
- Menstrual cups, which are small plastic cups inserted like a tampon
- (click here to learn about how to use these options!)
If your period is not normal or unmanageable– for example, your flow is so heavy you need to change your pad/tampon every hour, your period or PMS prevents you from doing your daily activities, or any of these reasons– you should see your doctor to get checked out.
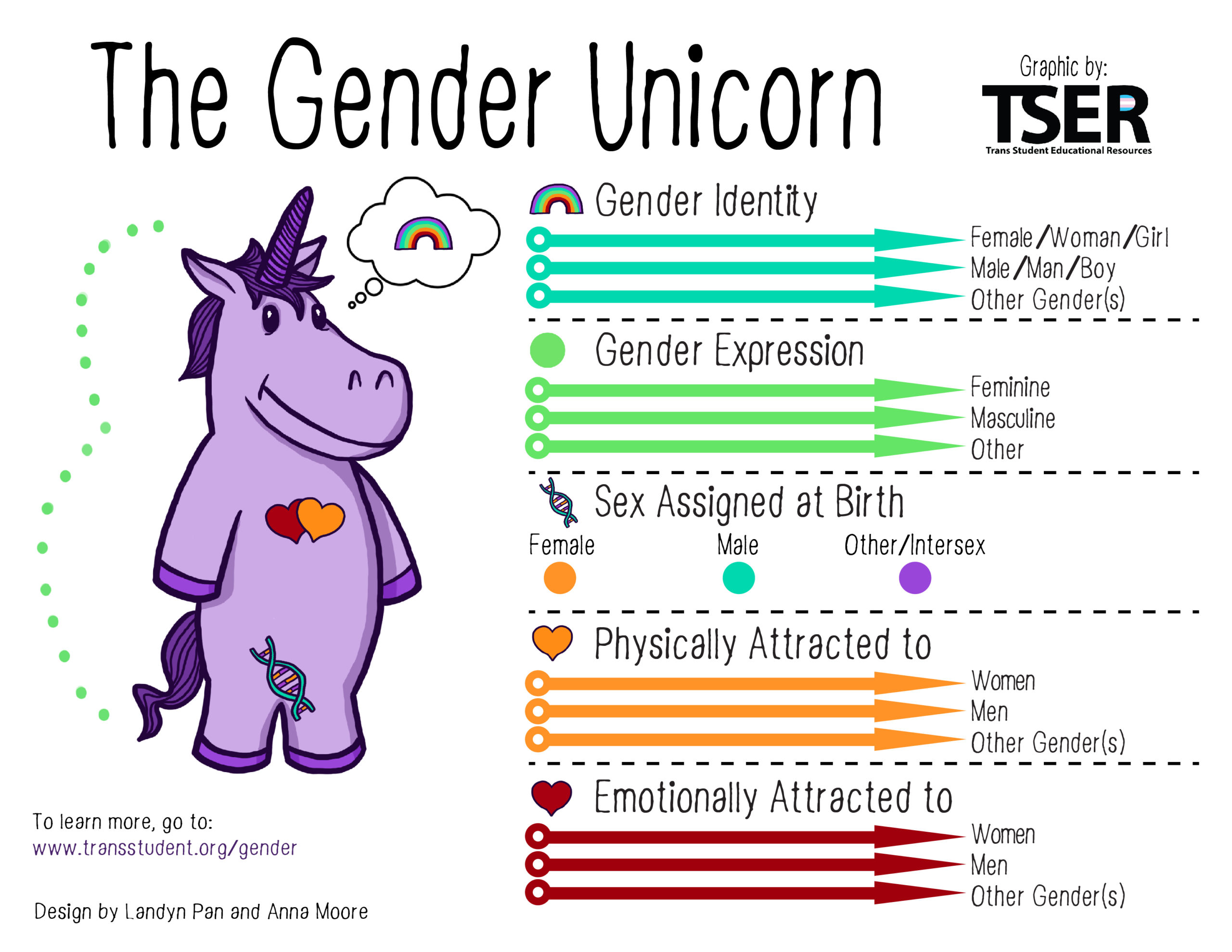
Sex, Gender, & Sexual Orientation
People often mix these three things up, so let’s define them!
Sex is assigned at birth and describes your external genital anatomy. For example, a baby born with a penis will be assigned male and a baby born with a vulva will be assigned female. Intersex describes those born with reproductive or sexual anatomy that doesn’t match what is typically assigned male or female. Learn more about what it means to be intersex here.
Gender identity is a person’s internal sense of their gender- whether they feel like a woman, man, neither, or both- and may or may not match their sex assigned at birth. Gender expression is how a person presents their gender to other people, like through clothes, voice, behavior, or other means.
Cisgender means that a person’s gender identity matches their sex assigned at birth.
Transgender means that a person’s gender identity does not match their sex assigned at birth. Some people who identify as transgender may take steps transition, such as through gender affirming hormone therapy or surgery, and others may not.
Sexual orientation describes who a person is attracted to. Straight describes those attracted to the opposite sex, gay describes men who are attracted to men, lesbian describes women who are attracted to women, and bisexual describes people attracted to men and women. However, these aren’t the only sexual orientations- there are lots! Learn more and find resources at the Trevor Project.
(Sources: NPR, Planned Parenthood)
A healthy relationship is one that makes you feel good: both partners are respectful, supportive, and are putting equal effort into the relationship. An unhealthy relationship does not make you feel good: one or both partners may be possessive, controlling, or manipulative, or pressure the other partner into doing things they don’t want to do.
On this page:
Signs of a Healthy/Unhealthy Relationship
Here are some signs of a healthy, unhealthy, and abusive relationship from Loveisrespect.org:
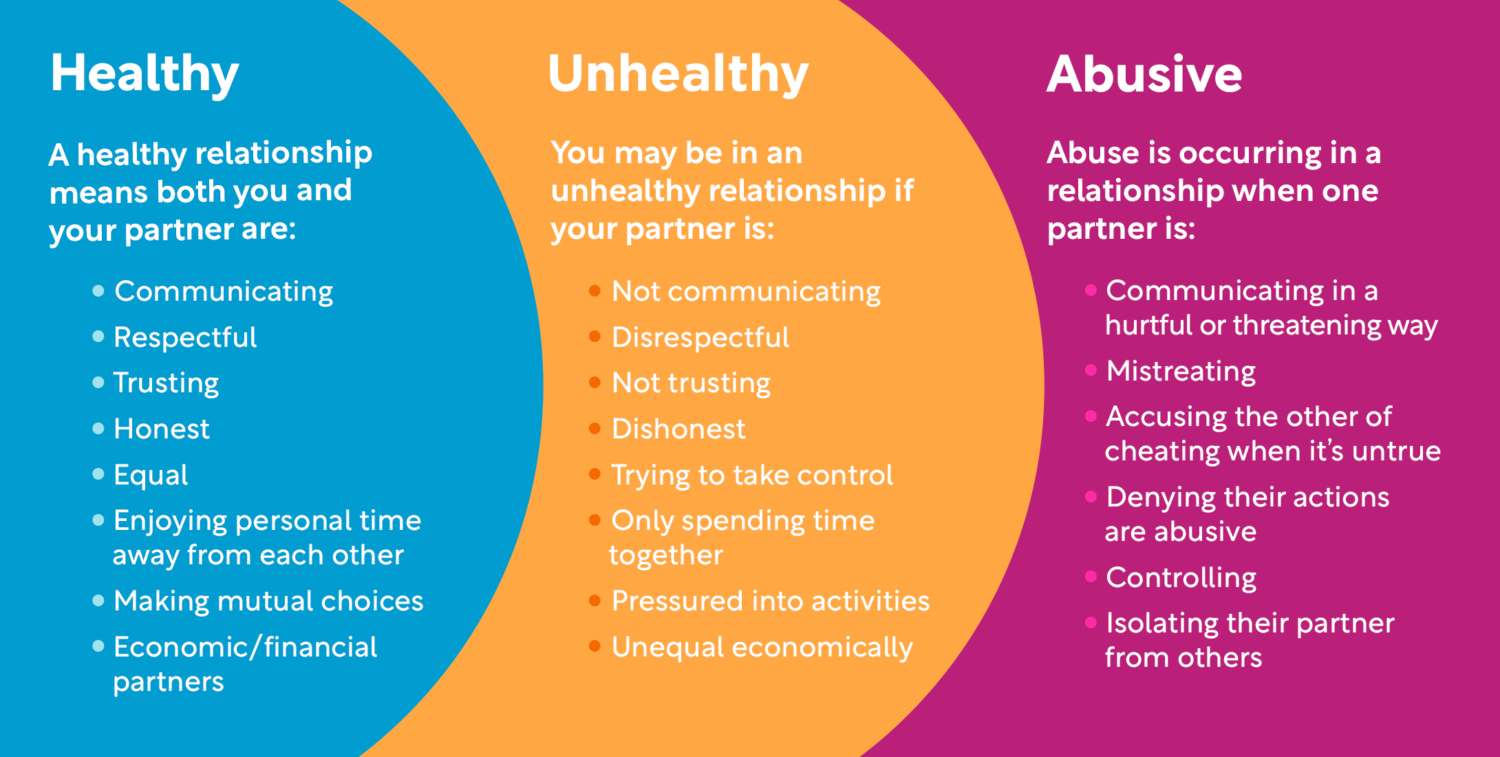
If you think you or a friend is in an unhealthy or abusive relationship, reach out to a parent or trusted adult, such as a teacher, coach or older sibling, for help. Hope Works is a great local resource for additional support.
If you think a friend is in an abusive relationship, here are some tips from One Love to help a friend in an abusive relationship:
- Start the conversation on a positive note, make your friend comfortable
- Be supportive
- Focus on unhealthy behaviors
- Don’t preach to your friend, they often don’t see themselves as victims
- Don’t blame friend
- Allow friend to make decisions for themselves
- Offer solutions
- Plan for more conversations
- For more support, call the National Domestic Violence Hotline: 1-800-799-7233
Healthy Relationships & Sex
It’s important that you feel comfortable communicating with your partner and setting boundaries—about the amount of time you’ll spend together, what you feel comfortable with telling your friends about the relationships, how you’ll handle disagreements, and about if/when/how you want to have sex. Because sex can be highly charged and hard to talk about, especially for young people, it is important to establish strong communication from the beginning.
If you don’t feel ready to have sex or simply don’t want to have it, that’s okay! Research shows that teens often perceive that their peers are having sex at higher rates than they actually are. This is important because these misperceptions can actually influence students’ behaviors: for example, students who believe that their peers are having more sex are more likely to have sex sooner than students who don’t think their peers are having more sex. So let’s discuss how many teens in Howard County have had sex. According to the 2018-2019 Youth Risk Behavior Survey, 21.2% of Howard County high schoolers have had sex. To break this down by grade, this number increases as students get older: 10.6% of 9th graders have had sex, and 35.7% of 12th graders have had sex. So if you’re a high schooler not having sex, you’re in the majority.
If you don’t want to have sex but your partner does, it is important to clearly communicate your boundaries. Your partner should always respect your boundaries without making you feel guilty or bad. If your partner is pressuring you to do anything sexual that you don’t want to do, here are a few different ways to handle the situation:
- If you feel safe, build the relationship: explain how you feel and why you don’t have sex. Listen to each other and discuss your needs and boundaries.
- Say no firmly using serious facial expressions. Create physical distance between you and your partner (for example, move away and cross your arms).
- Delay and remove yourself from the situation. Say you have to go to the bathroom and text a friend to pick you up, or say your parents said you have to go home.
- Avoid the situation by suggesting public or group settings to hang out in, such as going to the movies with friends.
(Source: Reproductive Health National Training Center)
Talking about Sex
Whether you are thinking about having sex with a partner, don’t want to have sex with a partner, or want more information and are thinking of asking a parent/trusted adult some questions, it’s important to be able to have open, safe conversations about sex.
Parents are a great resource, whether you want to ask questions about relationships or need help making a doctor’s appointment to get on birth control, but not all parents may be open to discussing sex with their child. Scarleteen offers some suggestions to gauge whether your parents would be open to this conversation, such as asking about a situation in a song or movie, or bringing up a friend (don’t make up a situation or your parent will think you’re talking about yourself). If you think your parents would be open to talking about sex with you, then here are some strategies to get the conversation started:
- If you want to gauge your parent’s reaction first, bring up a situation in a movie or TV or something that’s going on with a friend (don’t make up a situation or your parent will think you’re talking about yourself) to get their ideas about sex before disclosing anything
- The car is a private place where you don’t have to make eye contact with your parent
- Write a text, email, or note if you don’t feel comfortable talking
Check out this Planned Parenthood video for more tips on talking to your parents:
If you don’t think that your parent would be interested in talking about sex, or if you think that they would have a negative reaction if you disclosed that you are thinking of having/having sex, try to find a different adult to talk to. It could be an older sibling, coach, teacher, school nurse, aunt or uncle, or anyone else in your life who you think could provide judgement free guidance. In Maryland, you do not need parental consent to get birth control, and at the Howard County Health Department services are free for those under 19. For more advice on talking to your parents, check out Scarleteen’s guide here.
With a partner, talking about sex can be hard for different reasons- maybe you don’t know what they’re comfortable with, or aren’t sure if you’re ready to have sex, or need to discuss birth control and safer sex but don’t know how to bring it up. It is important that you and your partner can communicate openly before, during, and after sex, and that you can tell your partner what you want, and feel comfortable saying no without receiving anger or guilt in return. Talking about sex is not a one-time thing, but should be openly discussed regularly to ensure that everyone is on the same page. Here are some strategies from Scarleteen on starting a conversation with your partner about sex:
- Pick a neutral spot to have the conversation (somewhere private, but maybe not while you’re undressed or already having sex)
- Use “I” statements (“I feel that” instead of “You make me feel that”)
- Acknowledge that it can be awkward- keep your sense of humor!
- Understand that sex is a sensitive topic and go into the conversation ready to be reaffirm your partner
- Use language that you both understand (for example, refer to oral sex using a name you both understand)
For more ideas, visit Scarleteen.
Consent is an agreement to participate in an activity. According to Planned Parenthood, sexual consent is an agreement to participate in a sexual activity, and must be:
- Freely given: consenting is a choice you make without pressure, manipulation, or under the influence of drugs or alcohol
- Reversible: anyone can change their mind about what they feel like doing, anytime. Even if you’ve done it before, and even if you’re both naked in bed.
- Informed: You can only consent to something if you have the full story. For example, if someone says they’ll use a condom and then they don’t, there isn’t full consent.
- Enthusiastic: When it comes to sex, you should only do stuff you WANT to do, not things that you feel you’re expected to do.
- Specific: Saying yes to one thing (like going to the bedroom to make out) doesn’t mean you’ve said yes to others (like having sex).

Consent doesn’t have to be scary or super formal- think of it as a check-in to make sure both people are feeling good! It also will look different for people that you have different relationships with. If this is your first time having sex with your partner, or if you’re new to sex in general, it’s a good idea to get verbal consent (for example, asking “Do you want to have sex right now?” and hearing a “Yes!” back). If you and your partner are in a long-term relationship and know each other very well, you might be able to understand their physical cues better (for example, pulling you closer as opposed to just sitting there). However, it’s important to note that even if you’ve had sex with someone before, once or 100 times, that each sexual act requires consent, every time you have sex.
Scarleteen created a resource called the “Yes/No/Maybe So: Just the list,” with a comprehensive list of things that you can decide if you want to consent to or not consent to during sex. It’s a great resource, especially if you go through it with a partner, so check it out!
(Source: Scarleteen)
What is NOT consent
There are some conditions under which a person cannot give consent. Sex without consent is rape or sexual assault. If a person is drunk, high, or asleep, is severely distressed or ill, or can’t understand what they’re saying yes to, then they cannot consent, and doing any sort of sexual act with them (not just penetrative intercourse) is sexual assault or rape. Having sex with someone who is much younger than you can also be considered sexual assault or rape (Source: RAINN).
Consent means that both partners have agreed to engage in a sexual act both freely and enthusiastically. If someone is being pressured, guilted, blackmailed (for example, if their partner threatens to reveal their sexual orientation), or fears any negative consequences from saying no, then they cannot give consent freely. If someone says no, it does not mean that they need to be convinced- it means that you need to stop what you’re doing and check to see if they’re okay.
This chart from Scarleteen shows what enthusiastic, freely given consent can sound like, and what nonconsent sounds like. Nonconsent will not always be a verbal “No,” but could rather be a lack of consent, and could be portrayed through words or body language. In other words, nonconsent is not always what someone says or does, but what someone doesn’t do or say.
Some common verbal signals of consent and nonconsent
What can consent sound like? | What can nonconsent sound like? |
Yes | No |
I’m so sure | I’m not sure |
I know | I don’t know |
I’m excited | I’m scared |
Dont stop! | Stop |
Whoohoo! Yippee! Hot damn! Zip-a-dee-doo-dah! | [silence] |
More! | No more |
I want to. | I want to, but… |
I’m not worried | Wait, I feel worried about… |
I want you/it/that | I don’t want you/it/that |
Can you please do… | Can you please not do… |
I still want to | I thought I wanted to, but… |
That feels good | That hurts |
Mmmmmmmm. | [silence] |
Yes | Maybe |
I love you and I love this | I love you/this, but… |
I want to do this right now, like this | I want to do this, but not right now/this way |
I feel good about this | I don’t know how I feel about this |
I’m ready | I’m not sure I’m ready |
I want to keep doing this | I don’t want to do this anymore |
[insert praise to your deity of choice here] | [no such praise] |
This feels so right | This feels wrong |
YES! | [silence] |
What To Do if Your Consent Is Violated
If you have been sexually assaulted or raped, know that it is never your fault.
In Howard County, HopeWorks is the organization that supports survivors of sexual assault. Visit their website to learn more about your rights and options. You can also call their 24 hour helpline at 410-997-2272 for immediate support.
After a sexual assault, it is important to protect yourself from pregnancy and HIV. The best option is to go to Howard County General Hospital, where they will offer you Plan B to prevent pregnancy, as well as post exposure prophylaxis (PEP) for HIV prevention. If you don’t feel comfortable going to the hospital, you can also get emergency contraception at a pharmacy or the health department and PEP for HIV prevention is available at Chase Brexton.
Folks who experience sexual coercion or assault often may need more than medical support– they may also need mental and emotional support. HopeWorks offers peer support, community, and crisis, ongoing, and group counseling for survivors.
Sexually transmitted infections or STIs, also called sexually transmitted diseases or STDs, are infections that you can get from vaginal, oral, or anal sex.
STIs such as chlamydia, gonorrhea, and syphilis are easily curable, but can cause more serious health problems if they go untreated. Others, such as HPV (human papillomavirus) and herpes, are treatable but cannot be cured. HIV (human immunodeficiency virus) is a more serious infection that requires lifelong treatment.
Young people are more likely to get STIs: in Maryland in 2019, 15-24 year-olds accounted for 13% of the population but 64% of chlamydia and 39% of gonorrhea cases (Source: MD Center for STI Prevention). The good news is that, with condom use, STI testing, and the HPV vaccine, we can prevent the spread of STIs.
On this page:
- What are STDs and How Are They Transmitted
- Common Signs & Symptoms
- STI Testing
- HPV Vaccine
- Condoms & Other Safer Sex Supplies
- Condom Distribution Program
- PrEP
What Are STDs and How Are They Transmitted (Planned Parenthood)
Common Signs & Symptoms
There are many different STIs that have different symptoms- if you want to learn more about the different STIs, check out Planned Parenthood for more. However, there are some common symptoms that may indicate that you have an STI:
- sores or bumps on and around your genitals, thighs, or butt cheeks
- unusual discharge from your vagina or penis
- burning when you pee and/or having to pee a lot
- itching, pain, irritation and/or swelling in your penis, vagina, vulva, or anus
- flu-like symptoms like fever, body aches, swollen glands, and feeling tired.
There are other things, like a urinary tract infection, that could cause some of these symptoms. But if you have any of these symptoms and have had vaginal, anal, or oral sex without a condom, get tested for STIs.
It’s important to note that many people who have STIs don’t have symptoms, or won’t have symptoms for a long time, but can still pass the infection to their partner. For this reason, it’s recommended that you get tested whenever you get a new sexual partner, not just when you experience symptoms.
STI Testing
The Howard County Health Department provides STI testing (all services are free for patients 19 and under). You do not need your parent’s consent to get tested for STIs, and if you come to the Health Department your parents will not be notified of your results. Call 410-313-7500 to make an appointment and visit our website to learn more.
At your appointment, the provider will ask you some questions about your sexual history- like how many partners you’ve had in the last three months, what types of sex you’re having, and how often you use a condom when you have sex- in order to determine which tests they will give you. The tests may require a urine sample, blood test, swab of the genitals, swab of the rectum, throat swab, or examination. If you are experiencing symptoms of an STI, the provider will give you an exam to get a better idea of what’s going on. After the appointment, if you have a positive test result the Health Department will give you a call within 7-14 days.
HPV Vaccine
One STI, HPV, is vaccine preventable! Some types of HPV, also known as genital warts, can lead to cervical cancer, as well as cancer of the vulva, vagina, throat, anus, or penis. The HPV vaccine, Gardasil 9, prevents infection from the 9 most disease-causing strands of HPV. The HPV vaccine is recommended for all people starting at the age of 11-12, but if you haven’t gotten it yet it’s not too late! The Howard County Health Department offers HPV vaccines for everyone ages 11-26.
Condoms & Other Safer Sex Supplies!
Condoms are the only method of birth control that can be used to prevent the transmission of STIs. However, they only work if you use them consistently and correctly. So let’s learn how to use them!
External Condoms
How to put on and take off an external condom:
 (Source: CDC)
(Source: CDC)
External condoms can be used for vaginal, anal, and oral sex. Lubricants, or lube for short, can be used with condoms not only to make more pleasurable, but to make condoms more effective! Lube decreases friction, which makes the condom less likely to tear. For oral sex, you can use flavored condoms and flavored lube as well!
Internal Condoms
How to insert and take out an internal condom:
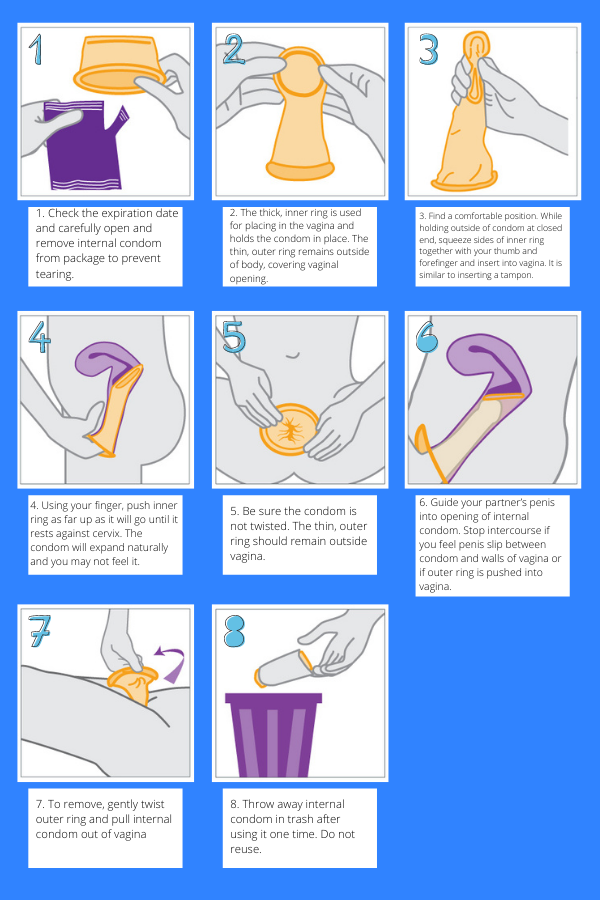 (Source: CDC)
(Source: CDC)
Internal condoms (sometimes known as “female condoms”) can be used for vaginal and anal sex. There are several reasons you may want to use them as opposed to external condoms: they can be inserted up to 8 hours before sex, the receptive partner (partner being penetrated) can control their condom use instead of relying on a partner, they offer additional STI protection on the vulva, and they feel different than external condoms.
To use internal condoms for anal sex:
- Check the expiration date and carefully open and remove internal condom from package to prevent tearing.
- Remove the inner ring from the condom. The outer ring remains outside of the body, covering the anus.
- Using clean hands, stick your fingers inside the condom and insert it into the anus, until the outer ring rests outside the body. Another option is to insert your partner’s penis into the condom, and then use your partner’s penis to guide the condom into place.
- Be sure the condom is not twisted and the outer ring remains outside the body. Stop intercourse if you feel the penis slip between the condom and the anus or if the outer ring is pushed inside the anus.
- To remove, gently twist the outer ring and pull internal condom out of the anus.
- Throw away internal condom in trash after using it one time. Do not reuse.
Dental Dams
How to use a dental dam:
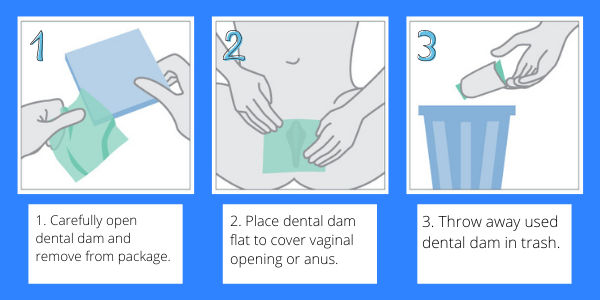 (Source: CDC)
(Source: CDC)
Dental Dams are used to protect against STIs when engaging in oral sex. They can be used with lube, flavored or unflavored, to make oral sex more pleasurable. Dental dams can only be used for one sexual act, and then must be thrown away. Make sure you don’t flip the dental dam over during sex, but make sure that you’re only touching one side, and your partner is touching the other, the entire time.
PrEP for HIV Prevention
The Howard County Health Department offers PrEP, pre-exposure prophylaxis, for HIV prevention. PrEP is a once-daily pill that can be up to 99% effective at preventing HIV through sex and about 70% effective at preventing HIV through drug injection. PrEP may be right for you if you have tested negative for HIV, have vaginal or anal sex without condoms, have a sexual partner with HIV, have had an STI in the past six months, or if you inject drugs with shared needles. Visit the CDC’s website for more information. The Howard County Health Department offers PrEP, visit our website or call 410-313-7500 to learn more!
https://www.youtube.com/watch?v=TR8-3uAuZGo[/embed
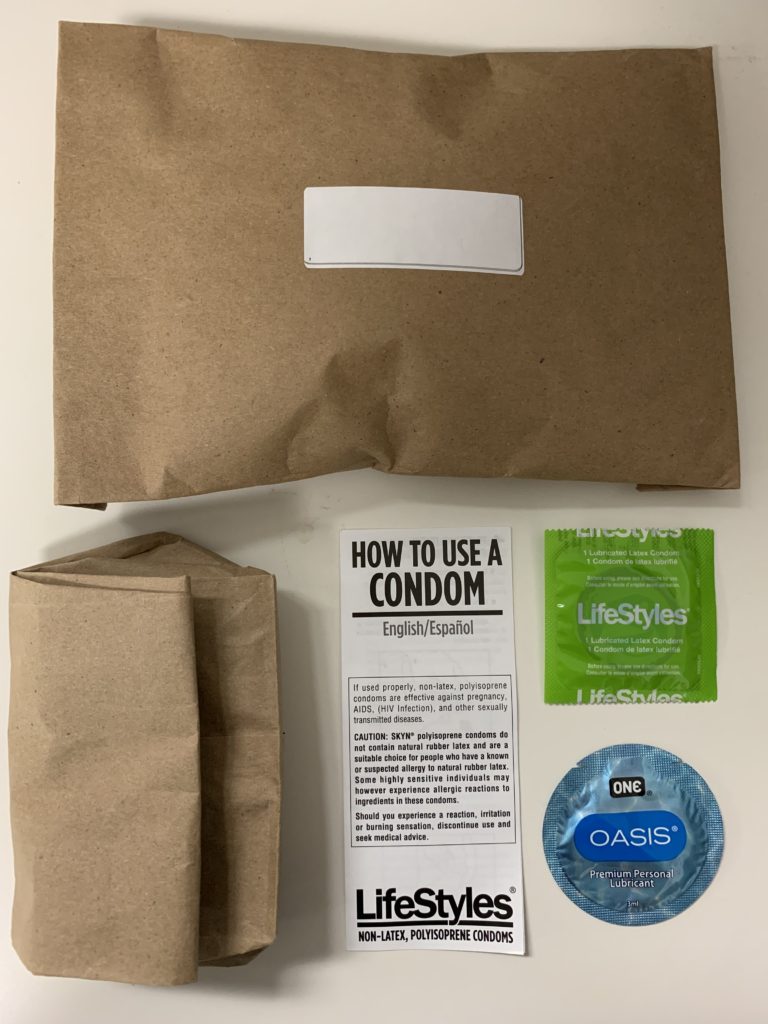
Condom Distribution Program
Fill out THIS FORM to order free condoms.
The Health Department offers FREE safer sex supplies, including condoms, lubricants, internal condoms, and dental dams, to all Howard County residents! Fill out this form and we will mail you the supplies you need in a discrete envelope, pictured below.
Birth control is an essential part of sexual health and family planning. It’s a great way to prevent pregnancy, regulate your periods, get relief from some conditions (such as endometriosis or acne) and, with barrier methods, prevent the transmission of STIs.
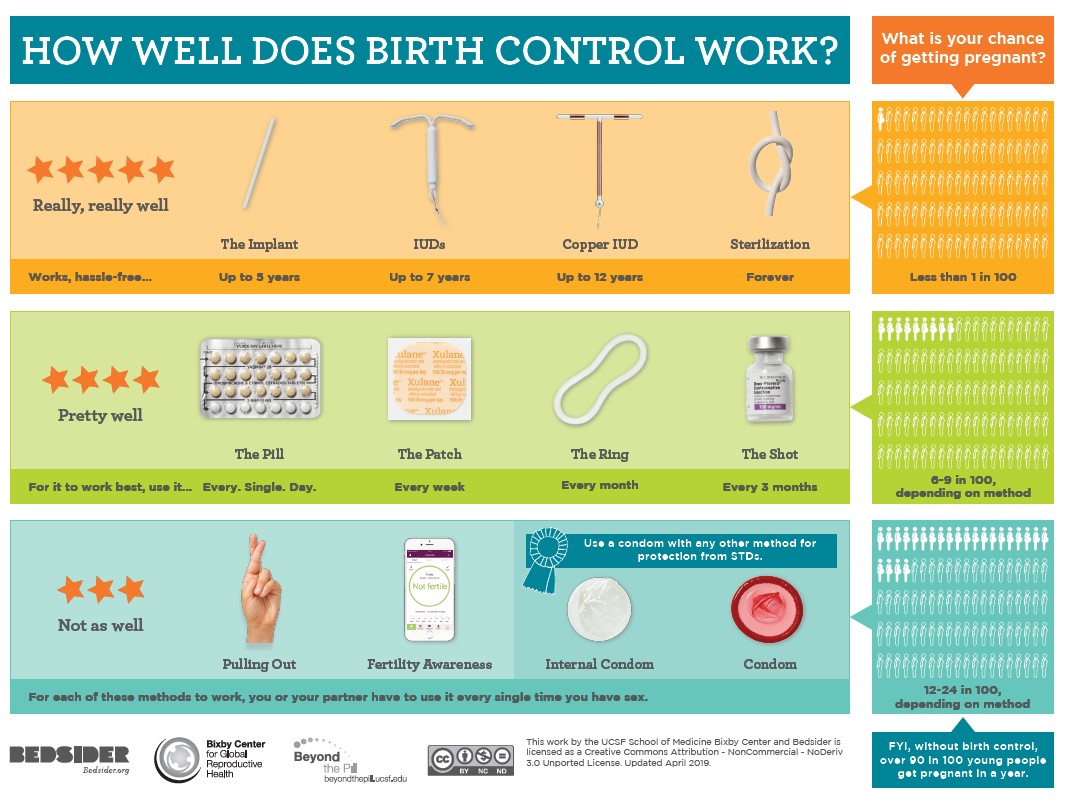
There are several different types of birth control, including types that are hormonal or non-hormonal. Abstinence is the only 100% sure way to prevent pregnancy, but if you’re having sex, there are lots of options that vary in effectiveness:
- The arm implant, the hormonal IUD (intrauterine device), and the copper (non-hormonal) IUD are 99% effective at preventing pregnancy.
- The pill, patch, ring, and shot are moderately effective, at about 91-94% effective with real use, although with perfect use (if you use them exactly as intended, with no mistakes ever) they can be 99% effective.
- Condoms are only 82% effective with real use, so we encourage you to use a more effective method of birth control with a condom to prevent both pregnancy and the transmission of STIs.
- Other less effective methods include the diaphragm, withdrawal, the sponge, spermicide, and fertility-based awareness.
To learn more about the pros and cons of each method, check out Bedsider and Planned Parenthood.
Emergency Contraception
What if the condom breaks, you forgot to take your birth control pill, or you have unprotected sex? Emergency contraception prevents pregnancy after unprotected sex. There are 3 types of emergency contraception:
- Plan B/Next Choice (Levonorgestrel-based pills)- pill that is 95% effective when taken within 24 hours of unprotected sex and can be up to 5 days after sex, but decreases in effectiveness each day, and is available over-the-counter (without a prescription). It is most effective for those who weigh under 155 pounds
- Ella– pill that is 85% effective and can be taken up to 4 days after unprotected sex, and is available with a prescription. It is most effective for those who weigh under 195 pounds.
- Copper IUD– intrauterine device that is 99.9% effective when inserted by a healthcare provider up to 5 days after unprotected sex, and can remain in place for up to 10 years
The Howard County Health Department offers emergency contraception. Call 410-313-7500 to learn more.
What to Expect During a Birth Control Visit at the Howard County Health Department
When visiting the Howard County Health Department to get a birth control method, here’s what you can expect. Once you check in with the front desk, a nurse will bring you into a clinic. They’ll ask you some questions about what is most important to you in a birth control method, go over the different options, and help you decide which is best for you. We will do our best to initiate your chosen method that same day, whether that is giving you a prescription for birth control pills, administering the Depo Provera Shot, or inserting an IUD or implant. Here at the Howard County Health Department, we want to make it as easy as possible to get your preferred method of birth control.
Services offered at the Howard County Health Department, Reproductive Health Clinic:
- Sexual/reproductive health education
- Preconceptual health counseling
- Gynecological exams
- Birth control choices
- Condom distribution
- Pregnancy testing
- Emergency contraception
- Breast exams and mammogram referrals
- Pap screening/colposcopy
- HPV vaccine
- Smoking cessation classes
- STI screening
- PrEP
- Expedited partner therapy
 There are many great local, state, and national resources around sexual and reproductive health. Here are some of our favorites.
There are many great local, state, and national resources around sexual and reproductive health. Here are some of our favorites.
Howard County Health Department – Reproductive Health
The Reproductive Health Clinic is open Monday-Thursday at 8930 Stanford Boulevard, Columbia MD. We see uninsured and underinsured patients, and services are free to those 19 and under. We always accept new patients. Call 410-313-7500 to make an appointment.
https://www.howardcountymd.gov/Departments/Health/Clinical-Services
HCPSS LGBTQIA+ Youth
HCPSS is committed to providing an educational and work environment that is free from discrimination, fosters equitable opportunities, and values diversity and commonality. You can learn more about the resources and support offered to students here: https://www.hcpss.org/supports/lgbtqia-youth/.
Chase Brexton POWER Clinic
Chase Brexton offers healthcare to everyone, insured and uninsured. The POWER Clinic (Protecting Ourselves With Every Resource) provides HIV and STI testing, PrEP, PEP, and HIV counseling and support.
410.837.2050
Chase Brexton Columbia: https://chasebrexton.org/locations/columbia
Hope Works
Hopeworks is the organization in Howard County that supports survivors of sexual assault and domestic violence. They offer a 24-hour helpline for sexual, dating, and domestic violence, residential services, counseling, advocacy, and legal assistance.
24 helpline: 410.997.2272
www.wearehopeworks.org
PLFAG Howard County
PFLAG Howard County supports the health and wellbeing of gay, lesbian, bisexual, and transgender people and their friends and family through support, education, and advocacy. They offer support groups, pro bono counseling, and resources.
Rainbow Youth Alliance
Supports the community of gay, lesbian, bisexual, transgender, intersex, queer, and questioning teens and their allies.
410.290.8292
http://rainbowyouthalliancemd.org/
Planned Parenthood of Maryland
A not-for-profit family planning agency that provides high-quality, affordable reproductive health care for women, men and teens.
410.576.1414
https://www.plannedparenthood.org/planned-parenthood-maryland
For general sex ed resources: https://www.plannedparenthood.org/learn
Bedsider
Allows users to compare birth control methods side-by-side in order to choose the option that’s best for you!
Scarleteen
An online resource geared towards teens and young adults for everything and anything related to sex- sexuality, gender identity, relationships and more.
Love is Respect
Offers support, information and advocacy to young people who have questions or concerns about their dating relationships. Free and confidential phone, live chat and texting services are available 24/7/365.
Chat at www.loveisrespect.org
Text loveis to 22522
Call 1-866-331-9474
http://www.loveisrespect.org/
Trevor Project
The leading national organization providing crisis intervention and suicide prevention services to lesbian, gay, bisexual, transgender, queer & questioning youth.
24/7 Lifeline: 866-488-7386
https://www.thetrevorproject.org/