Mental health includes our emotional, psychological, and social well-being, and determines how we make choices, handle stress, and relate with others. People with “good” mental health don’t always feel happy or never feel lonely, but rather have the tools to cope with stress, trauma, and adversity.
Mental health is an essential part of overall health, and interacts with physical health in many ways. For example, some mental illnesses increase the risk of physical conditions (for example, depression increases the risk of stroke) and some chronic health problems can increase the risk of mental illness. It is important to take your mental health as seriously as you take your physical health.
What is mental illness?
Mental illnesses are conditions that affect a person’s thinking, feeling, mood, or behavior, and may impact a person’s daily functions and their ability to relate with others. They can be short term, episodic (on and off with clear starting and ending points), or long-lasting. They are not caused by one single factor, but are influenced by:
- Biological factors, like genes or brain chemistry
- Life experiences, such as trauma or abuse
- Family history of mental health problems
Mental illnesses are NOT caused by weakness, laziness, or any other moral failing. It is not your fault if you have a mental illness. The good news is that mental illness is treatable, just like a physical illness, and recovery is possible. If you think you (or someone you know) might have a mental illness, it is best to consult a professional as soon as possible. A health care professional will connect the symptoms and experiences you are having to help formulate a diagnosis.
Mental Illness Among Adolescents
Mental illness is very common among adolescents and young adults: 1 in 5 young people suffer from a mental illness. Being a teenager is an overwhelming time– your body and brain go through physical changes, you must navigate new social environments, and you are expected to take on increasing responsibilities at school and at home. For many, these pressures and problems can lead to one or more of a variety of mental health conditions. It is around this age that many mental health conditions develop: around 50% of lifelong mental illnesses begin by age 14 and 75% begin by age 24.
If you are experiencing feelings of sadness or hopelessness, you are not alone. According to Maryland data from the Youth Risk Behavior Survey, in Howard County in 2022-2023:
- 31.9% of high school students reported feeling sad or hopeless in the past year
- 30.5% of middle school students reported feeling sad or hopeless in the past year
Warning Signs of Mental Illness
If you think you, or someone you know, may have a mental health condition, it’s important to know and recognize the 10 common warning signs that you should seek help.
- Feeling very sad or withdrawn for more than two weeks.
- Seriously trying to harm or kill oneself or making plans to do so.
- Severe out-of-control, risk-taking behaviors.
- Sudden, overwhelming fear for no reason.
- Not eating, throwing up or using laxatives to lose weight; significant weight loss or weight gain.
- Seeing, hearing or believing things that are not real.
- Repeated usage of drugs or alcohol.
- Drastic changes in mood, behavior, personality or sleeping habits.
- Extreme difficulty in concentrating or staying still.
- Intense worries or fears that get in the way of daily activities.
If you are experiencing one or more of these symptoms, find a trusted adult and reach out for help. Remember, your mental health is as important as your physical health and you deserve to get help and feel better. There are many different mental health conditions that affect people in different ways. For a breakdown of symptoms, treatments, and resources for different conditions, check out the National Alliance of Mental Illness.
Sources: MentalHealth.gov, Help Guide
In a Crisis
Finding Mental Health Support
If you are in a non-crisis situation, there are many ways you can get support. The first is to reach out to a trusted adult. Whether that is a parent or guardian, teacher, coach, faith leader, or anyone else, it is important to let that person know that you (or a friend) need help.
If you are experiencing mental illness, you deserve to get help and feel better, but it is not always easy to ask for help. For some ideas on how to start this conversation with a trusted adult, read Mental Health America’s guide to asking for help.
Once you have connected with your trusted adult, there are several steps that you can take together.
- Talk to your primary care provider or PCP (your regular doctor, nurse practitioner, or physician’s assistant). Your PCP can help you understand the feelings and symptoms you are experiencing and can refer you to a mental health professional.
- Take advantage of school-based mental health services. The Howard County Public School System (HCPSS) has school counselors, school psychologists, and school social workers to support its students. If you are interested in utilizing these resources, contact your student services office (find your school’s website, then go to “Student Services” or “Staff” to find a staff member to reach out to). For more information, check out the HCPSS website here.
- Find a mental health professional. Finding a team of professionals to support your recovery is essential to getting better. Your primary care provider is a great place to start in connecting you to the care you need. Below are some tips to help you connect to a mental health professional in Howard County:

Coordinate with your family’s health insurance. With your parent/guardian’s help, figure out what mental health services are covered by your plan, if you need a referral from your PCP, and identify in-network providers. For more information on this process, visit the Resources for Adults page.
Find a professional in Howard County. Here is the Howard County Youth Behavioral Health Directory. 
This is a list of licensed counselors, social workers, psychologists and psychiatrists in Howard County that serve teens. This directory contains information on the services each practice provides, the forms of insurance they take, and which languages they offer. Here are some helpful definitions to help you navigate the directory:
- Outpatient treatment– The patient is not admitted to stay overnight at a hospital or clinic; for example, going to an appointment with a doctor or therapist
- Psychiatrist— A doctor with special training in the treatment and diagnosis of mental conditions; can prescribe medication but usually can’t provide therapy
- Psychotherapy— The therapeutic treatment of mental illness, sometimes called “talk therapy,” wherein feelings, thoughts, and behaviors are explored; there are many types of psychotherapy, like cognitive behavioral therapy, dialectical behavior therapy, ect.
- Psychologist— Has an advanced degree in psychology, can diagnose mental conditions and provide individual and group therapy
- Insurance– This describes how the provider accepts payment. For example, if it lists “Medicare, Medical Assistance, Blue Cross Blue Shield, Cigna” the provider will accept payment from those programs or companies. Below are more terms used to describe payment methods.
- Self-pay– You pay the provider directly, instead of going through an insurance company.
- Sliding-fee scale–Providers set the price of their services based upon the financial situation of their patients. If you cannot afford a provider’s normal fee but they have listed “sliding-fee scale” for insurance, they are willing to work with you to accommodate your financial ability.
- In-network– The provider contracts with an insurance company and provides care to its clients; those with private insurance will pay less to visit an in-network provider than an out-of-network provider. For example, if a provider lists “Blue Cross Blue Shield” for insurance in the directory, they are an in-network provider for that company.
- Out-of-network– The provider does not have an “in-network” relationship with insurance companies, but insurance companies will reimburse you for a portion of the cost of their services. For example, if you visit an out-of-network provider, you may pay the therapist’s fee up front, and your insurance company will later reimburse you for a certain percentage of the cost.
- Evidence-based practice— Methods of treatment that are supported by research, clinical expertise, and patient characteristics; Cognitive Behavioral Therapy and Dialectical Behavior Therapy are examples of evidence-based treatment options
The Howard County Network of Care for Mental/Behavioral Health is another way to find a mental health professional. The Network of Care is an online information portal of community health services, substance use treatment programs, and resources for people with developmental disabilities. Click this link to search for providers offering Adolescent/Youth Counseling by zip code!
CAREAPP is a search tool that can help connect you to community programs and services for mental health support, health, education, employment assistance and more. You can download the phone app or visit findhcresources.org.
Sources: National Alliance on Mental Illness, American Psychological Association, Centers for Medicare and Medicaid Services

Levels of Care for Mental Health Treatment
For a more detailed account of treatment options, what to expect when accessing mental health care, and how to advocate in a crisis, please see the Navigating A Mental Health Crisis booklet from the National Alliance on Mental Illness.
Outpatient Psychotherapy
Individual psychotherapy involves regularly scheduled sessions between the person and a mental health professional. Psychotherapy is a form of treatment that can help children and families understand and resolve problems, modify behavior, and make positive changes in their lives. There are several types of psychotherapy that involve different approaches, techniques and interventions. At times, a combination of different psychotherapy approaches may be helpful. In some cases, a combination of medication with psychotherapy may be more effective.
It is important that parents and caregivers are closely involved in their child’s treatment. The child may have therapy sessions alone with the therapist. At times, parents and caregivers may participate in therapy sessions with their child or may have private therapy sessions with their child’s therapist.
Remember that due to confidentiality laws, the therapist may not be able to share everything you child tells the therapist in therapy. This can be very frustrating to parents and caregivers! Be sure to ask your child’s therapist what information they will share with you and what they cannot share with you.
Detailed explanations of different therapeutic modalities, including cognitive behavior therapy (CBT), dialectical behavior therapy (DBT) and interpersonal therapy, can be found here. For information on what to expect when exploring psychotherapy, check out Treatment Facts for Families from Children’s Mental Health Matters.
Psychoeducation
Psychoeducation teaches people about their illness and how they’ll receive treatment. Psychoeducation also includes education for family and friends where they learn things like coping strategies, problem-solving skills and how to recognize the signs of relapse. Family psychoeducation can often help ease tensions at home, which can help the person experiencing the mental illness to recover. Many of NAMI’s education programs are examples of psychoeducation, which can be located here: https://namihowardcounty.org/.
Self-Help And Support Groups
Self-help and support groups can help address feelings of isolation and help people gain insight into their mental health condition. Members of support groups may share frustrations, successes, referrals for specialists, where to find the best community resources and tips on what works best when trying to recover. They also form friendships with other members of the group and help each other on the road to recovery. As with psychoeducation, families and friends may also benefit from support groups of their own.
Outpatient Psychiatry
Psychiatry can be provided by psychiatrists or psychiatric nurse practitioners. Psychiatrists have a medical degree and at least four additional years of study and training. They provide medical/psychiatric evaluations and a full range of treatment interventions for emotional and behavioral problems and psychiatric disorders. As physicians, psychiatrists can prescribe and monitor medications. Psychiatric or mental health nurse practitioners can provide assessment, diagnosis and therapy for mental health conditions or substance use disorders. In Maryland, they are also qualified to prescribe and monitor medications. For more information on mental health providers, visit the website here.
Psychiatric Rehabilitation Programs (also called Psychosocial Rehabilitation)
Psychiatric Rehabilitation Programs (PRPs) are licensed under COMAR 10.63. Individuals are eligible for PRP services, both at the day program site (on-site) and in their living arrangement or other community setting (off-site) if: 1) they receive Medical Assistance (MA), 2) are diagnosed with a serious mental illness that meets the state’s priority population, and 3) meet the medical necessity criteria established for this service. PRPs provide services to help people develop the social, emotional and intellectual skills they need in order to live happily with the smallest amount of professional assistance they can manage. Psychosocial rehabilitation uses two strategies for intervention: learning coping skills so that they are more successful handling a stressful environment and developing resources that reduce future stressors.
Treatments and resources vary from case to case but can include medication management, psychological support, family counseling, vocational and independent living training, housing, job coaching, educational aide and social support.
Structured Outpatient Programs
Unlike outpatient therapy sessions, structured outpatient provides a more comprehensive treatment experience. These programs have detailed schedules that use a variety of therapeutic techniques, such as cognitive behavioral therapy, group process therapy and even holistic practices, like yoga or meditation. Structured outpatient is often used as the next step after inpatient treatment or as a preventative measure before a person needs a higher level of care. There are two types of programs – Intensive Outpatient and Partial Hospitalization. IOP and PHP can be beneficial for motivated clients with stable home environments, as clients in IOP or PHP are able to return home each night.
Structured outpatient also provides more direction in an individual’s treatment. With traditional outpatient counseling, it is the client’s responsibility to complete assignments between sessions and apply recovery skills they’ve learned. In IOP or PHP, the individual has extra support from clinicians and fellow participants. They spend more time at the treatment center, which allows them to focus their attention on recovery.
For individuals who are not managing a condition effectively at the outpatient level, or who do not meet the criteria for inpatient, structured outpatient can be the ideal treatment situation. They can receive a higher level of care than weekly outpatient sessions while still maintaining their normal living situation. Structured outpatient is opening up new possibilities and better treatment outcomes for those who have tried other levels of care and are looking for the next step. For more information on Structured Outpatient Programs, visit the website here.
Intensive Outpatient
IOP typically consists of at least six hours each week for adolescents and nine hours each week for adults.
Partial Hospitalization
PHP consists of at least 20 hours each week. Partial hospitalization provides care and monitoring for a person who may be having acute psychotic symptoms without being a danger to self or others. It allows a person to return home at night and is much less disruptive. It can also be used as a transition from inpatient hospital care before a complete return home.
Residential Rehabilitation Programs
Residential Rehabilitation Programs (RRPs) are licensed under COMAR 10.21.22. Residential beds are targeted to those individuals served by the public behavioral health system who are diagnosed with a serious mental illness and need assistance/support services to live in the community.
Priority for placement in RRP is given to individuals returning to the community from State inpatient hospitalizations and individuals who are diagnosed with a mental illness and are homeless. All referrals for residential placement are screened by the Howard County Health Department/Bureau of Behavioral Health/LBHA to assure that the referral meets the criteria for placement.
Contact Jocelyn Tillman, HCHD Child, Adolescent and Transitional-Aged Youth Care Coordinator at jtillman@howardcountymd.gov or 410-313-3367 for more information.
Residential Treatment Centers
In Maryland regulation, a “residential treatment center” (RTC) is a psychiatric institution that provides campus-based intensive and extensive evaluation and treatment of children and adolescents with severe and chronic emotional disabilities who require a self-contained therapeutic, educational, and recreational program in a residential setting. Next to inpatient psychiatric hospitalization, an RTC is the second-most restrictive and costly treatment for children and adolescents. For more information, visit the Maryland Coalition of Families site located here.
Crisis Stabilization Units
Crisis Stabilization Units (CSU) are small inpatient facilities of less than 16 beds for people in a mental health crisis whose needs cannot be met safely in residential service settings. CSUs may be designed to admit on a voluntary or involuntary basis when the person needs a safe, secure environment that is less restrictive than a hospital. CSUs try to stabilize the person and get him or her back into the community quickly.
The Child and Adolescent High Acuity Residential Crisis Program at Brooklane caters to individuals aged 8 to 17 in behavioral or mental health crises, offering the resources of the hospital without the inpatient psychiatric setting. The average stay is lengthier than the inpatient setting, as it is designed to assist in establishing permanent resources, offer ongoing educational services and contribute to long-term healing.
Inpatient Hospitalization
There may be times when a person is admitted to the hospital for intensive treatment. Private psychiatric hospitals, general hospitals with a psychiatric floor or state psychiatric hospitals are designed to be safe settings for intensive mental health treatment. This can involve observation, diagnosis, changing or adjusting medications, ECT treatments, stabilization, correcting a harmful living situation, etc.
If a person and their doctor agree that inpatient treatment is a good idea, they will be admitted on a voluntary basis, meaning that they choose to go. Some private hospitals will only take voluntary patients.
If a person is very ill and refuses to go to the hospital or accept treatment, involuntary hospitalization is an option. The legal standard for an involuntary hospitalization requires that a person be considered a “danger to self or others.” This type of hospitalization usually results in a short stay of up to 3 days but can occasionally last a week or so longer.
Before a person is discharged from the hospital, it is important to develop a discharge plan with a social worker or case manager. Family members should be involved in discharge planning if the person is returning home or if they will need significant support. A good discharge plan ensures continuous, coordinated treatment and a smooth return to the community. For more information on forms of hospitalization, visit the website here.
Suicide is a serious public health problem that affects many young people. Suicide is the second leading cause of death for youth between the ages of 10-14 and third leading cause of death for youth ages 15-24 (CDC, 2020).
Suicidal thoughts, much like mental health conditions, can affect anyone regardless of age, gender or background. In fact, suicide is often the result of an untreated mental health condition. However, the majority of people with mental illness will not die by suicide.
What are the risk factors?
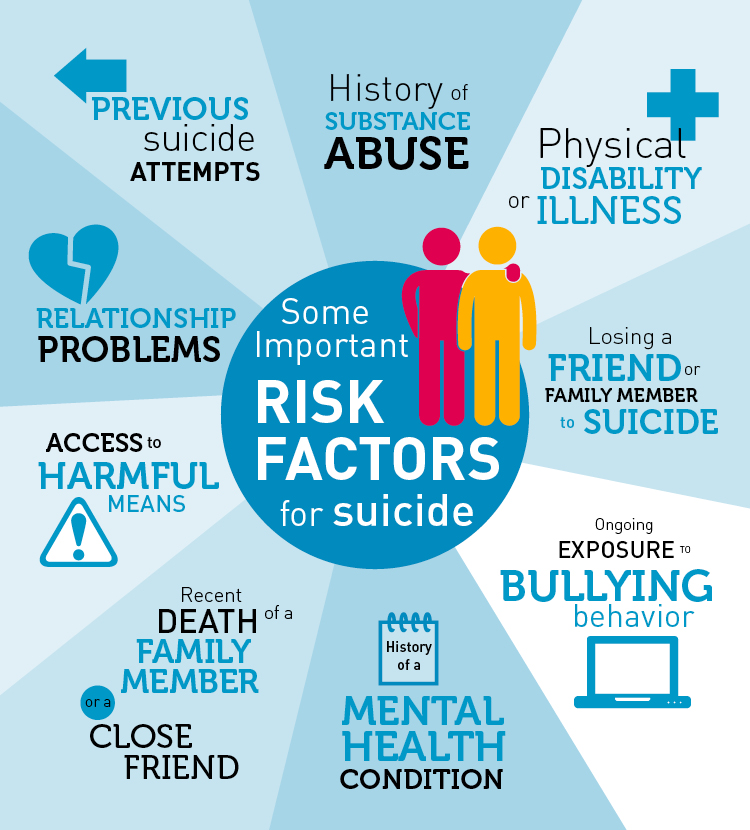
Risk factors are issues in a young person’s life that increase the likelihood (risk) of them acting on suicidal thoughts. There are a number of things that may put a person at risk of suicide, including:
- A family history of suicide.
- Substance abuse – Drugs and alcohol can result in mental highs and lows that exacerbate suicidal thoughts.
- Intoxication – More than one in three people who die from suicide are found to be currently under the influence.
- A serious or chronic medical illness.
- Serious mental health conditions – Depression, anxiety disorders, bipolar disorder, and personality traits of aggression, mood changes, and poor relationships.
- Gender– Although more women than men attempt suicide, men are four times more likely to die by suicide.
- A history of trauma, abuse, and/or neglect.
- Prolonged stress.
- Age– People under age 24 or above age 34 are at a higher risk for suicide.
- A recent tragedy or loss.
What are the warning signs?
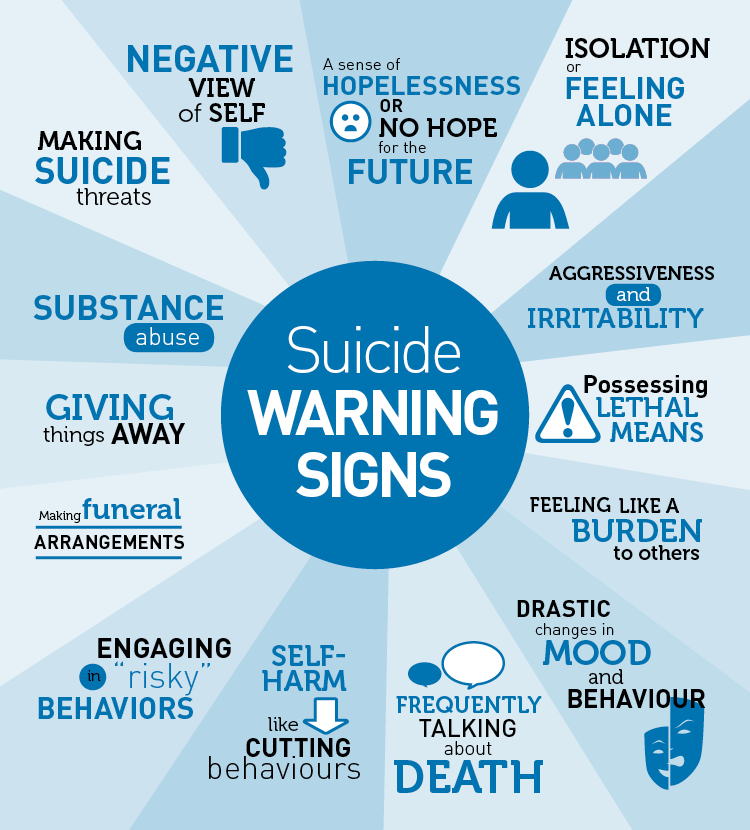
Warning signs indicate that someone may be thinking about suicide. If someone you know is showing one or more of these signs, don’t wait- get help immediately. It is especially important to get help if someone is exhibiting these behaviors in connection to a painful change, loss, or event. These warning signs include:
- Talking about wanting to die or to kill oneself
- Looking for a way to kill oneself
- Talking about feeling hopeless or having no reason to live
- Talking about feeling trapped or in unbearable pain
- Talking about being a burden to others
- Increasing the use of alcohol or drugs
- Acting anxious or agitated; behaving recklessly
- Sleeping too little or too much
- Withdrawing or feeling isolated
- Showing rage or talking about seeking revenge
- Displaying extreme mood swings
If you see these signs in yourself or someone else, reach out to someone you trust, a parent, friend, teacher, coach, or religious leader right away.
You can contact the National Suicide and Crisis Lifeline by calling or texting 9-8-8.
You can also contact the Grassroots Crisis Intervention 24-Hour Crisis Hotline. Call at 410-531-6677 or visit www.grassrootscrisis.org for more information.
What are the protective factors?

Risk factors can be balanced out to a certain extent by the presence of protective factors. There are a range of protective factors that can help to reduce suicidal behavior, including:
- Strong, positive relationships with parents and guardians – feeling secure and supported
- Connections to other adults– teacher, coach, pastor, counselor
- Closeness to caring friends
- School safety
- Feeling a sense of belonging to something bigger than themselves – community, culture, religion, sports team
- Resilience
Sources: American Foundation for Suicide Prevention, CDC, MentalHealth.gov

Did You Know…
Asking about suicidal thoughts or feelings won’t push someone into doing something self-destructive. In fact, offering an opportunity to talk about feelings may reduce the risk of acting on suicidal thoughts.
It is important to know how to start the conversation about suicide, what to say during the conversation, and how to seek help.
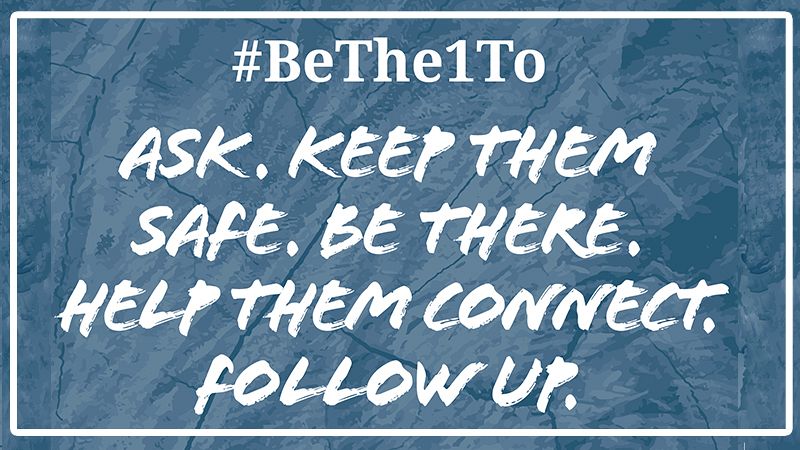
Starting the Conversation
First find a private place to talk where there will not be any distractions. Set aside time to have a conversation and find a comfortable place to sit.
Remember to approach the situation with care and with open ears. If you do not know what to say, try one of these opening lines:
- “I’m worried about you and would like to know what’s going on so I can help.”
- “Are you okay? I noticed that you’ve missed school/practice a few times.”
- “It seems like something is bothering you. Do you want to talk about what’s going on?”
- “Seems like you haven’t been yourself lately. What’s up?”
During the Conversation
It is important to give full attention to the individual when they are being open about how they are feeling. Remember to:
- Keep it casual and relax. Think of the conversation as a chat, not a therapy session.
- Listen carefully.
- Avoid fixing the problem for them.
- Ask open-ended questions to help them talk instead of responding with “yes” and “no.”
Let them open up at their own speed. Do not demand answers or force them to say anything that they are not ready to.
Get Help
Assist the individual with getting the professional help that they need.
- Call or Text 9-8-8
- Press 1 to reach the Veterans Crisis Line
- Press 2 to connect to a trained Spanish-speaking crisis counselor.
- Press 3 for to reach specialized crisis services for the LGBTQI+ community.
- Help them connect: assist with reaching out to a parent, teacher, counselor, hotline, or other mental health professional.
- Contact Grassroots Crisis Center Hotline: 410-531-6677.
Don’t give up. Stay available and keep offering help. Handle their trust with care. Follow up and keep checking in to see how they are doing.
For more tips on how to start the conversation, ask questions, listen, and connect to resources, check out Seize the Awkward.

Today’s youth are navigating social and emotional development, the complexities of the digital world, discrimination, and challenges from the COVID-19 pandemic. For many young people, these issues can contribute to mental and emotional distress. Access to unsecured firearms for youth at risk can result in suicide, serious injury, or violence towards others.
According to the Maryland Vital Statistics Administration, between 2003 and 2020, 35% of suicides among Marylanders under the age of 25 were by firearm. Suicide rates have been rising for decades, particularly among youth. Suicide is complex but often preventable. Along with safely storing firearms, knowing the warning signs can save a life.
Resources:
- Safeguard Your Home: A guide to help prevent suicide
- Firearm Safe Storage and Youth Suicide Prevention (Maryland Department of Health)
- Firearm Safe Storage Guide (Maryland Department of Health)
- Firearm Safe Storage Guide (Spanish)
- Firearm Safe Storage Brochure (Maryland Department of Health)
- Firearm Safe Storage Brochure (Spanish)
- Extreme Risk Protective Orders: A Health Intervention to Reduce Gun Violence
- Extreme Risk Protective Orders: A Health Intervention to Reduce Gun Violence (Spanish)
- Maryland Safe Storage Map

Self-harm and self-injury are any forms of hurting oneself to cope. Sometimes, when people self-harm, they do not do so as a suicide attempt. Rather, they self-harm as a way to release painful emotions. The 988 Suicide & Crisis Lifeline provides 24/7 Talk, Text, and Chat support.
Common Types of Self-Harm
Self-harm can manifest differently for everyone. And, the ways people may self-harm extend far beyond the usual news media references such as cutting. Simply, self-harm is anything and everything someone can do to purposely hurt their body.
Here are some of the most common types of self-injury:
- Cutting
- Scratching
- Burning
- Carving words or symbols into the skin
- Hitting or punching oneself (including banging one’s head or other body parts against another surface)
- Piercing the skin with sharp objects such as hairpins
- Pulling out hair
- Picking at existing wounds
Recognizing the Signs of Self-Harm
Stigma creates shame and embarrassment, making it hard for people who self-harm to get help. So, look out for yourself and for your pals. If you suspect that someone in your life is self-harming, here are some warning signs to keep top of mind:
- Scars
- Fresh cuts, burns, scratches, or bruises
- Rubbing an area excessively to create a burn
- Having sharp objects on hand
- Wearing long sleeves or long pants, even in hot weather
- Difficulties with interpersonal relationships
- Persistent questions about personal identity
- Behavioral and emotional instability, impulsiveness, or unpredictability
- Saying that they feel helpless, hopeless, or worthless
Crisis Text Line can help you deal with self-harm. Text a Crisis Counselor at 741741.
Why Do People Self-Harm?
Let’s start with this: everyone needs a way to cope with their emotions. People who self-harm have turned to hurting themselves as their coping mechanism to manage their emotions.
So, people might self-harm to:
- Process difficult emotions
- Distract themselves from their negative feelings
- Feel something physical, particularly if they are feeling numb
- Develop a sense of control over their lives
- Punish themselves for perceived faults
- Express emotions that they are unable to share
How to Cope With Self-Harm
Emotions can be really painful sometimes. It’s totally normal to need ways to cope with and process the hard things in your life. If you are using self-harm to manage your emotions, we’re here for you. And, we want to help keep you safe.
Here are some ways to push through, process, and cope with your emotions.
- Talk someone you trust or a counselor to help you cool down – 988 Suicide & Crisis Lifeline
- Meditate or breathe deeply
- Talk to a professional
- Understand what influences your self-harm
- Replace harmful behaviors
- Address underlying emotions
- Build a support system
Resources:
- How to Cope with Self Harm (Crisis Text Line)
- Self-Harm (Johns Hopkins Medicine)
- Cutting & Self-Injury (kidshealth.org)
- How Can I Help a Friend Who Cuts? (kidshealth.org)
- What Can I Do If My Friend is Cutting Themself? (American Academy of Pediatrics)
- 988 Suicide & Crisis Lifeline
Source: Crisis Text Line

Crisis Resources
 Grassroots Crisis Intervention (Crisis/Suicide/Runaway/Shelter)
Grassroots Crisis Intervention (Crisis/Suicide/Runaway/Shelter)
Grassroots operates a 24-hour crisis intervention and supportive counseling hotline. Callers may remain anonymous and may call for a variety of reasons including suicide, family and relationship problems, shelter needs, violent or threatening domestic situations, loneliness or depression, and chemical dependency issues, among others. The Hotline is available 24 hours a day, seven days a week.
8990 Old Annapolis Rd., Suite A, Columbia, MD 21045
410.531.6677
 988 Suicide & Crisis Lifeline
988 Suicide & Crisis Lifeline
The Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals.
English/240+ additional languages: 9-8-8
Deaf or Hard of Hearing: Use your preferred relay service or dial 7-1-1 then 9-8-8 or visit the website for the chatline.
- Dial 988, Press 1 to reach the Veterans Crisis Line
- Dial 988, Press 2 to connect to a trained Spanish-speaking crisis counselor.
- Dial 988, Press 3 for to reach specialized crisis services for the LGBTQI+ community.
 The Trevor Line
The Trevor Line
Crisis intervention & suicide Prevention for LGBTQ Youth
24/7 Hotline: 1-866-488-7386. Visit the website for chat and text options.
Howard County Resources
Howard County Health Department Behavioral Health Navigation Referral
Need help finding a therapist, psychiatrist, substance use treatment provider, or other behavioral health resources? Fill out this online form. A Behavioral Health Navigator will help you decide which services best meet you need, connect you to community services and resources, and follow-up on the outcome of the referral.
Youth Behavioral Health Directory
A list of behavioral health providers that serve youth in Howard County. Go to How to Get Help for tips on navigating this guide.
CAREAPP
CAREAPP is a search tool that can help connect you to community programs and services for mental health support, health, education, employment assistance and more. You can download the phone app or visit findhcresources.org.
 Howard County Network of Care
Howard County Network of Care
A resource for individuals, families and agencies concerned with behavioral health. Regardless of where you begin your search for assistance with behavioral health issues, the Network of Care helps you find what you need – it helps ensure that there is “No Wrong Door” for those who need services.
 NAMI Howard County
NAMI Howard County
NAMI Howard County welcomes your call to help you find local resources and access mental health services. NAMI offers free peer support groups for people living with mental illness and their loved ones, as well as free education programs.
9650 Santiago Road, Suite 1
Columbia, MD 21045
(410) 772-9300
 The Horizon Foundation
The Horizon Foundation
As the largest independent health philanthropy in Maryland, the Horizon Foundation works to improve health and wellness for everyone who lives or works in Howard County. The Horizon Foundation offers mental health grant opportunities, an annual Mental Health Film Festival, and additional advocacy efforts. Check out their Emotional Support Human campaign for ways to check in on the mental health of your loved ones.
10221 Wincopin Circle, Suite 200
Columbia, MD 21044
410-715-0311
Suicide Prevention Trainings
If you want to learn more about suicide prevention, mental health, how to ask a friend if they are thinking about suicide, and what to do in a crisis, attend a suicide prevention training. There are many different programs for youth, family members, and community members, and many are offered to Howard County residents for free! For more information, check out trainings hosted by the Mental Health Association of Maryland or visit Grassroots Crisis Intervention Center’s Trainings webpage.
National Resources
![]() National Alliance of Mental Illness (NAMI)
National Alliance of Mental Illness (NAMI)
The nation’s largest grassroots mental health organization, NAMI has great resources about mental health conditions, warning signs and symptoms, treatments, peer support networks, as well as platforms for education and advocacy.
 Active Minds
Active Minds
Active Minds is a national leader in youth mental health advocacy and suicide prevention, with chapters at high schools and colleges across the country (including in Howard County! ). Visit their website for resources about mental health conditions, warning signs and symptoms, getting help, and how to help a friend. Visit your high school’s website or ask the student services office to see if your school has an Active Minds chapter and get involved!
 American Foundation for Suicide Prevention (AFSP)
American Foundation for Suicide Prevention (AFSP)
AFSP is a national voluntary health organization that empowers people affected by suicide through research, education, and advocacy. Visit their website for resources for those with mental conditions, survivors of suicide, and to learn about their advocacy efforts.
The Steve Fund is dedicated to supporting the mental health and emotional well-being of young people of color.
 MentalHealth.gov
MentalHealth.gov
Provides one-stop access to U.S. government mental health information, with specific resources for young adult
If you are concerned about the mental health of a young adult in your life, here are some resources to help you start a conversation and get connected to help. If you or someone you know is in immediate danger, call 911, 988, Grassroots Crisis Intervention Center at 410-531-6677 or visit the Resources for Teens page for more options.
 Howard County Department of Health Bureau of Behavioral Health
Howard County Department of Health Bureau of Behavioral Health
Visit the website to explore the Bureau of Behavioral Health’s resources, programs and services, and to get connected to help. If you need help finding a therapist, psychiatrist, substance use treatment provider, or other behavioral health resources for yourself or a family member, fill out the HCHD Behavioral Health Navigation Services online form.
 988 Suicide & Crisis Lifeline
988 Suicide & Crisis Lifeline
The Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals.
English/240+ additional languages: 9-8-8
Deaf or Hard of Hearing: Use your preferred relay service or dial 7-1-1 then 9-8-8 or visit the website for the chatline.
- Dial 988, Press 1 to reach the Veterans Crisis Line
- Dial 988, Press 2 to connect to a trained Spanish-speaking crisis counselor.
- Dial 988, Press 3 for to reach specialized crisis services for the LGBTQI+ community.
The CARE Line for Howard County Families
Child and Adolescent Resources and Education (CARE) for Howard County Families is a free service provided by the Howard County Office of Children and Families, with the support of Howard County Department of Community Resources and Services, the Howard County Local Children’s Board, Maryland State Department of Education, Howard County Mental Health Authority and the Governor’s Office for Children. The CARE Line is a resource and referral service for behavior issues, special needs, mental health concerns, adolescent concerns, support groups, and more. Call 410-313-CARE (410-313-2273) or email: children@howardcountymd.gov. Visit the website for more information.
 The Jed Foundation: What To Do if You’re Concerned About Your Teen’s Mental Health
The Jed Foundation: What To Do if You’re Concerned About Your Teen’s Mental Health
JED is a nonprofit that protects emotional health and prevents suicide for teens and young adults. This conversation guide covers signs that your teen may need help, how to prepare for the conversation, what to do and say during the conversation, what to do if your teen refuses help, and how to follow up after the conversation.
 Maryland Coalition of Families (MCF)
Maryland Coalition of Families (MCF)
MCF helps families that care for someone with behavioral health needs by helping them navigate services and systems, giving them tools to advocate, and connecting families to each other. Visit the website to get one-to-one support through an MCF Family Peer Support Specialist.
 NAMI Howard County
NAMI Howard County
The Howard County affiliate of the National Alliance on Mental Illness offers support and education programs, as well as advocacy and stigmafree campaigns. Visit the website to join their support group for parents and caregivers of children and teens with a mental health issue.
 Consumer Guide to Understanding Your Health Insurance Coverage for Mental Health and Substance Use Disorders
Consumer Guide to Understanding Your Health Insurance Coverage for Mental Health and Substance Use Disorders
This guide by the Maryland Insurance Administration provides tips for selecting a health insurance plan, how to work with your insurance company during mental health emergencies, how your health plan works, and your rights when your health insurer will not pay for health care services.
 Maryland Health Connection
Maryland Health Connection
Maryland’s official insurance marketplace, where you can compare and shop for plans, apply for Medicaid and the Maryland Children’s Health Program and more.
What Parents Can Do to Protect Children’s Mental Health During Remote Learning – A Statement from the Chief Medical Officer of the American Foundation for Suicide Prevention, Dr. Christine Moutier, on actions we can take to support the mental health of children.
Resources for Parents Following a Suicide Attempt – This resource guide compiles information related to safety considerations, local resources, and tools to assist parents in transitioning their child home from inpatient treatment.
For a calendar of upcoming community events, click here. To request community-based trainings, presentations, materials, & information, contact Jessica Fisher.
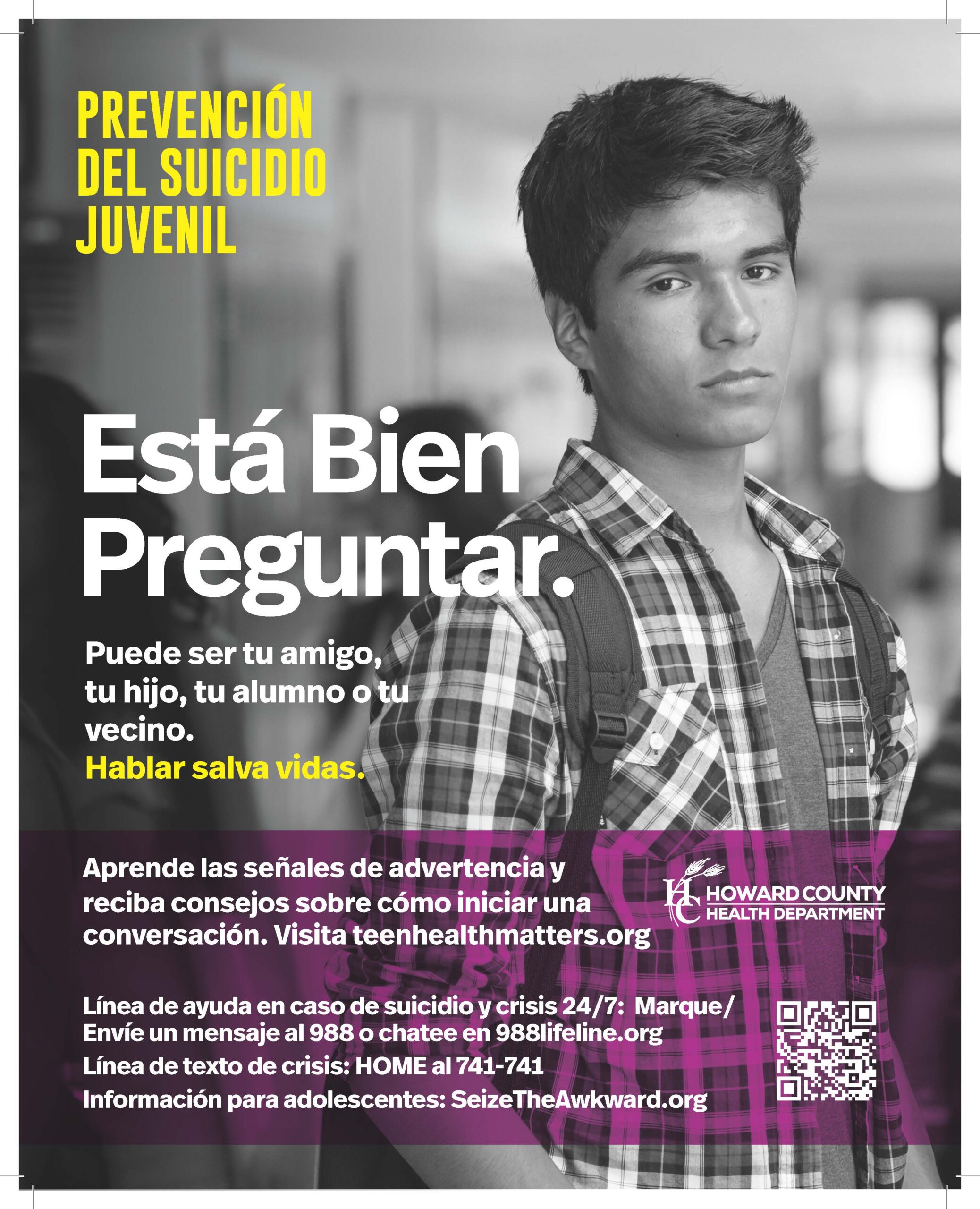
It’s Ok to Ask Campaign
It’s Ok to Ask is a suicide prevention campaign that aims to promote help-seeking behaviors and encourage conversations about mental health between family and friends. The QR codes on each of the images connect community members with resources on the Howard County Health Department Suicide Prevention webpage. For questions about the campaign, or to request materials, email Jessica Fisher at jefisher@howardcountymd.gov.
It’s OK to ask for help. It’s OK to ask a loved one about their mental health. Talking saves lives.
What is Sources of Strength?
 Sources of Strength is a peer leadership program where peer leaders and adult advisors are trained to design and share Hope, Help, and Strength-based messages with other youth in the community. The program aims to prevent suicide, bullying, and substance use by promoting help seeking behaviors and developing relationships with trusted adults.
Sources of Strength is a peer leadership program where peer leaders and adult advisors are trained to design and share Hope, Help, and Strength-based messages with other youth in the community. The program aims to prevent suicide, bullying, and substance use by promoting help seeking behaviors and developing relationships with trusted adults.
Joining the Team
Why become a Sources of Strength Peer Leader?
- Build leadership skills, interpersonal skills, and student connections
- Use your voice, and social influence to prevent suicide
- Learn how you can be a mental health advocate in the community
How does Sources of Strength work?
- Creates an interactive peer leadership program that influences positive social change
- Empowers students to create networks of connection and resiliency
- Increases help-seeking behaviors
- Promotes positive connections between peer leaders and adults
Want to see our past work? View campaigns from previous years here.